Project planning is the beginning of formal product development process, wherein the identified team enters a design control process that complies with medical device regulatory requirements (in the United States, per the FDA) and business strategy. This phase is all about determining the resources, the timing, and the work that’s required for product success.
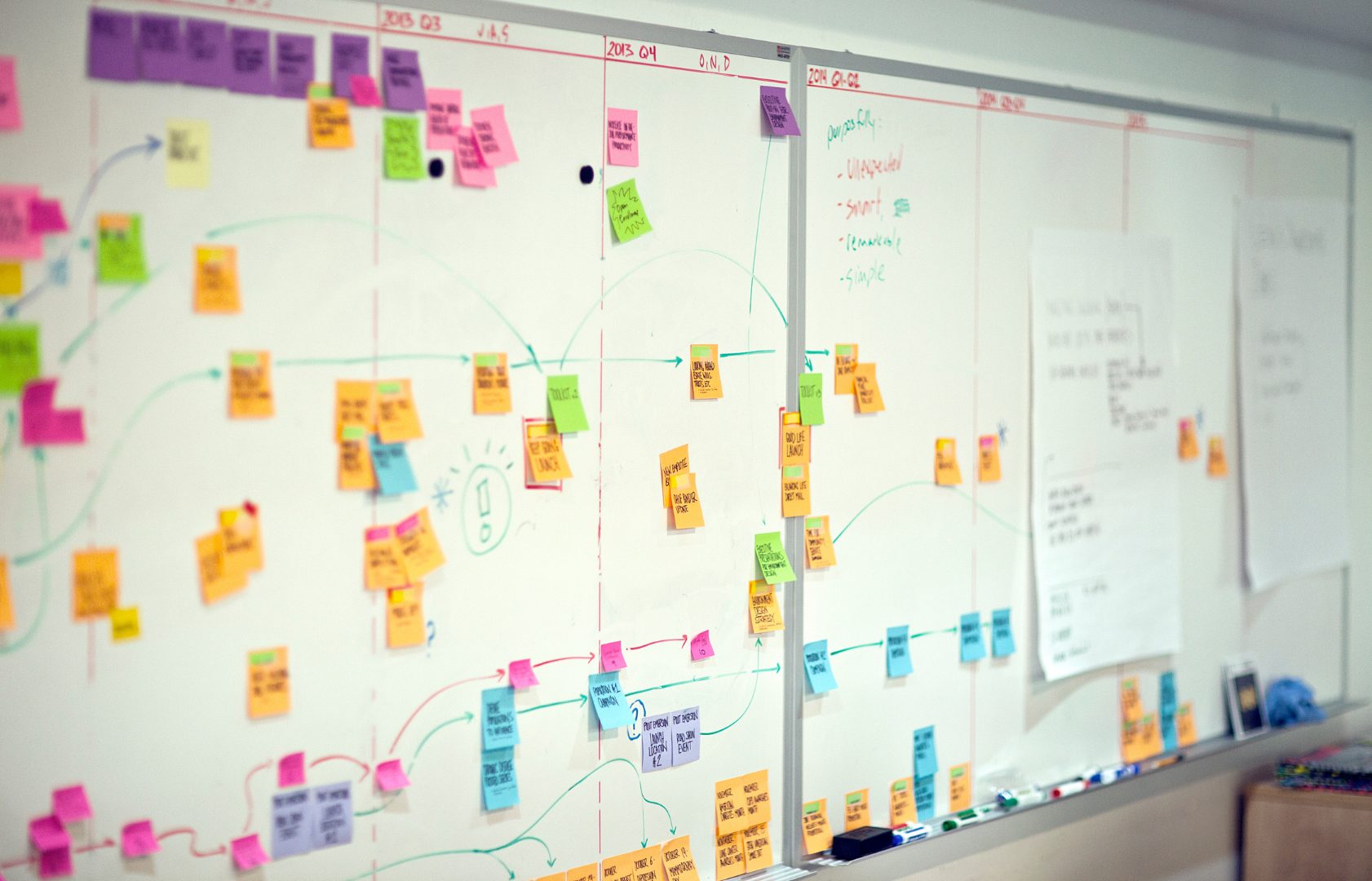
Robust planning lays out the tasks, timelines, and resource requirements for the project. The plan acts as the project “trail map,” guiding the project team as they “climb the mountain” on the same path to reach the “summit” safely together.
Where does preclinical work find its way into project planning for new medical technologies? What are the top considerations for preclinical work in this early development stage? GCMI Preclinical Program Director Evan Goldberg shares his insights below.
Product Overview and Design Concept
What are the different components in the product, and how does someone use it? What does the design look like – at the level of detail in between a napkin sketch and the final blueprints? When does preclinical work need to answer ‘how does someone use it?
“The key preclinical questions to ask and answer here are, what tests will the device or technology need to pass, and who will perform them? How many parts or test articles will you need to complete verification and validation testing in a preclinical environment? Surgical instruments or devices with complex delivery systems need to be tested in a cadaveric or in-vivo model to ensure they work as intended and designed.
“In many devices or technologies, preclinical work is the only way to identify and address potential mis-uses or risky design features and test worst case scenarios.”
Project and Regulatory Plans
What international standards does the device need to meet? What documents need to be completed at different points during product development? Will this product need approval from the FDA and/or a clinical trial?
“For FDA Class II devices, preclinical testing requirements vary widely, especially when it comes to GLP studies. Some technologies in this class require GLP studies, some do not. Consult the experts early in planning to determine a preclinical budget, ask for a pre-submission meeting with a representative of the appropriate regulatory body (FDA in the United States) to define your requirements early.
“For Class III devices, regulatory bodies including the FDA require proof of safety, possibly efficacy, biocompatibility and survival durations up to as many as 6 months or longer.”
Project schedule and budget
When will the project reach major milestones? What are the detailed steps to completing and testing the design, and in what order will they happen? What timeline risks are lurking?
“Preclinical testing needs for Class II devices vary widely. Many surgical instruments or devices must be tested in an acute model for performance and/or safety evaluation and that’s it. For other Class II devices like orthopedic implants, preclinical testing requirements are more timely and costly as they must be implanted in an in-vivo model with six month survival to prove safety and efficacy.
“Preclinical testing always takes more time and money than innovators think. You must prepare and budget for multiple types and rounds of testing including feasibility and biocompatibility which may require changes to a technology’s design based on information gathered in those studies.
“Class III devices frequently require 12 months or more in preclinical work. For implantables that are life saving or sustaining, regulatory bodies require survival studies with histology. Survival studies alone can take six months or more to complete. Histology and reporting take time to satisfy GLP requirements, not to mention prior proof of concept and feasibility testing in the validation process.
“Most importantly, know that the most expensive and time consuming study is the one you have to do twice. Evaluate your prospective preclinical partners carefully.
“Talk to experts early. Pad your numbers. Know that your team’s efforts will not go precisely to plan the first time. There will be iteration, repetition and additional requirements depending on results from verification and validation testing. A GLP study estimate alone is not enough to take to an investor for preclinical work. On the other end of that spectrum, in some cases it might not even be required.
“Budget, plan for and conduct pilot studies where errors or adjustments cost significantly less than in a GLP study. For 510K technologies, the cost of preclinical testing can range from the tens of thousands to hundreds of thousands of dollars. It is common for class III devices preclinical studies to be several hundred thousand dollars, not including proof of concept or feasibility studies. Again, evaluate and audit your prospective preclinical partners carefully.”
A trusted partner for any phase of your medical technology’s path to commercialization Our team knows the value of answering key questions to increase the odds of “summiting the mountain” safely together. GCMI serves as your comprehensive project planning, research and development team, taking an integrated view of product strategy and design. Our phased approach gives promising technologies the best chance to achieve commercialization in a cost efficient manner. And our industry leading preclinical CRO is a core contributor to our customers’ success.
“If we worked with another design and development firm, we wouldn’t have had the flexibility to do what we needed to do in the time frame we set. GCMI is unique in that we were able to choose the services that we needed precisely at the time we needed them. The way GCMI engages with their customers is unlike any other firm.”
“A good preclinical partner must be able to adapt to the needs, schedule and budget for a specific project. T3 Labs, now part of GCMI, has been an outstanding partner in supporting ALung throughout many preclinical studies. Preclinical work is always filled with unexpected outcomes – some good, some bad. Having a trusted preclinical partner that has the experience, expertise, and flexibility to work with your specific product, team, timeline and budget is of the utmost importance.”
– Jeremy Kimmel, PhD, Vice President of New Technologies for ALung